Imaging has come a long way in recent
years, but there remains a middle ground between physical examination and
MRI - light transillumination. I regularly use a penlight in the office
as a low tech but often helpful diagnostic tool. Tumors fall into four
groups based on opacity relative to surrounding tissues:
|
| Click on each image for a larger picture |
| Case 1: Mass arising a year after nail bed excision and skin graft for nail bed squamous cell carcinoma. |
 |
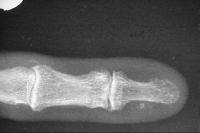
| Xrays show discrete calcification in the area, consistent with heterotopic ossification. |
 |
| Transillumination appearance, dark or opaque. |
 |
| Case 2: Firm mass arising just distal to the PIP joint, fixed to deep structures. |
 |
| Xray shows a contour change of the middle phalanx deep to the tumor. |
 |
| Transillumination is indeterminate, slightly darker than surrounding tissues. |
 |
| Intraoperative finding: classic giant cell tumor, arising from the PIP collateral ligament. |
 |
| Case 3: Painless dorsal middle phalanx mass. |
 |
| A standard plastic disposable flashlight is fine, but better if the tip is wrapped in opaque electrical tape to limit the light flare through the sides of the flashlight. |
 |
| Bright transillumination confirms the diagnosis of ganglion cyst. Treatment: observation. |
 |
| Case 4: similar to case 3. |
 |
| Flashlight |
 |
| A picture of the illumination is more obvious with the finger placed on a lit transparency light box. |
 |
| Case 5: illustrating the use of transillumination even in the darg skinned patient. Chronic dorsal distal phalanx tumor and concave nail deformity: |
 |
 |
| Flashlight: |
 |
| Transillumination: clearly a mucous cyst. |
 |
| Intraoperative excision and joint debridement, demonstration of the deep pull out sutures used to close the deep skin layer of an eponychial splitting incision: |
 |
| Healed. |
 |
| Search for...
tumor transillumination |
Case Examples Index Page | e-Hand home |