Clinical Examples: Thenar Flaps
| Fingertip
amputations remain a common problem with many treatment
options ranging from simple to complex. One of the more
useful regional flaps is the thenar flap, detailed in this
classic article (pdf file). The thenar flap
provides an excellent tissue match of color, texture,
bulk and contour of the lost finger pulp. The donor site
is inconspicuous and often provides fingerprints to the
new fingertip. This is a geometrically demanding
procedure and requires proper planning and attention to
detail. If planned as a transposition flap, the donor
site can be closed primarily. Concept and use are
presented below. |
| Click on each image for a larger picture |
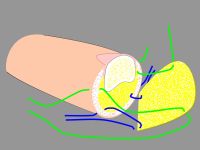
| A key issue is orienting the base of
the flap so that the flap comes to lie perpendicular
to the recipient site. This is best planned
in reverse using a template. This is helpful to also
plan the orientation change resulting from donor site
closure. |
| In this design,
The donor defect is closed as a transposition flap,
making best use of transverse skin laxity in this
area. This rotates the final flap orientation. |
| Click on the image
below to view the animation of the repositioning effect of
donor site closure: |
| The goal is to
position the flap against the recipient bed without
tension or torsion. In addition to proper alignment, two key points are: ¤ Adduct the thumb basal joint to bring the flap to the finger to reduce flap tension. ¤ Flex the finger MCP joint to reduce PIP flexion. |

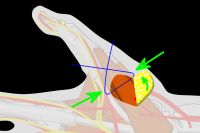
| Four corner
sutures may be all that is required. ¤ Strong (2-0 or 3-0) sutures should be used to secure these anchoring points. ¤ Avoid multiple sutures or tight closure. ¤ Avoid sutures in the base or tip of the flap - only suture the sides. ¤ The palmar finger skin edge should come to rest against the deep surface of the flap. Flap division is simpler if the palmar finger heals to the flap rather than to the donor site skin edge abutting the base of the flap. |
Top
| Case
1. 65 year old woman sustained a palmar oblique amputation of the middle fingertip in a closing garage door 10 days earlier; failure of composite tip replacement as a graft. |
| Flap elevation and
donor site closure. |

| Flap inset,
bringing the thumb to the finger. |


| Ideally, the flap
protrudes beyond the tip, providing extra skin which
will recontour to a rounded tip. |


| Six weeks later,
one month after flap division. |


| Result at one
year. |

| Donor defect. |

| Excellent contour
and new fingerprints. |


Top


| Because of the
length required, a proximally based flap was planned
as a trapezoidal flap, allowing Limberg flap style
closure. |

| Closure. |


| One month after
flap division. |




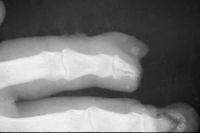
| The final result
was compromised by bone loss. The initial bone loss
was severe enough to warrant bone graft, but this
was contraindicated by the recent infection. |

| Over time, loss
of this structural support led to shortening and a
hook nail deformity. |

| Result at one
year. |

| Despite this, an
excellent resurfacing of the large defect has been
achieved. |


Top
| Case
3. This gentleman sustained partial amputations of all fingers in an industrial press. His index finger was the only digit with a potentially salvageable fingertip. |

| Distal phalanx
fracture stabilization. Pins were placed to protrude
proximally in anticipation of flap cover. |


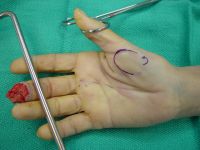
| Flap design. |

| Esmach bandage was
used as a template to plan a flap of optimum size and
position . |

| Inset. |


| One month after
flap division and hardware removal. |

Top
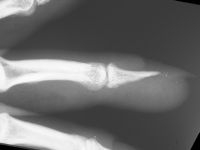
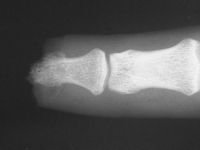
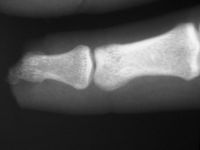
| Case
4. A dog bit off this young man's index fingertip. Although the PA Xray looks as though the bone was kept, additional views show an amputation through the tuft. |

| The defect. |

| Flap design. |

| Inset, using
Gelfilm® (no financial interest) as a nail bed
dressing. |


| Immediately prior
to flap division. |

| Result at six
weeks. The bulbous flap "biscuit deformity" due to
scar contracture at the flap junction, which was
corrected later with small Z-plasties. |

Top

| An ulnarly based
flap was used. |


| Trapezoidal donor
site closure on the proximal radial aspect of the
flap. |

| Excision of the
scarred skin and neuromas in continuity. |

| Flap inset. |


| Two layers of
immobilization were used. First, tape is placed
without tension to secure the thumb to the recipient
finger. |

| This was further
immobilized in a two piece plaster cast. The base cast
supported the thumb in adduction, but left the dorsal
view of the surgery exposed. This exposed area was
covered with a free strip of plaster held on with tape
to create a removable protecting cover. |

| In a cooperative patient with an adequate bandage, such rigid immobilization is not needed. |

| Result at three
months. |


| Case
6. This 72 year old man sustained a crush amputation of his right middle fingertip with exposed bone. |


| Flap design. |

| Fingertip defect. Note the skin graft on the dorsum of the middle phalanx: donor site for a cross finger flap to an index fingertip amputation years before by another surgeon. |

| Result six months
postop. |



| Result ten years
postop. |



| Transfer of
fingerprints depends on whether or not the donor area
has any. In this case, not. |

| Donor defect. |

Top
|
Final caveats and
take home points:
|
| Search
for... thenar flap fingertip amputation
|
Case Examples Index Page | e-Hand home |